In ophthalmology, every surgical day runs on tight schedules and tighter margins. A single missed clearance, outdated allergy list, or unconfirmed plan can ripple across an entire surgical block. This derails case flow, wastes staff time, and frustrates patients.
Yet for many ASCs, surgical coordination still relies on a fragile mix of paper packets, spreadsheets, email threads, and verbal updates. Staff manually re-enter data between systems. Tasks are tracked in silos. And coordination depends more on memory and hallway conversations than on system reliability.
This isn’t just inefficient. It’s unsustainable.
Table of Contents
The Cost of Surgical Inefficiency
Surgical days should run on precision, but for many ophthalmology practices, they run on patchwork. Coordinators print out paper forms. Nurses check with the front desk about clearances. Surgical techs search email threads or spreadsheets for missing information.
These manual workarounds aren’t just inefficient—they create risk. The disconnect between systems forces staff to double-check what should already be clear, slowing down patient flow and increasing pressure across the board.
In ophthalmology, where surgical volume is high and timelines are tight, the margin for error is slim. Each denied surgical claim can cost $300–$600 to rework. With a 5–10% denial rate due to documentation issues, these inefficiencies have real financial impact.
Where Current Systems Fall Short
Most ASCs use a combination of EHRs, spreadsheets, paper packets, and phone calls to coordinate care. These systems rarely talk to each other. When data needs to be shared, it’s re-entered manually or confirmed verbally—introducing errors.
- This fragmentation means:
- No single source of truth for the surgical schedule
- Staff forced to track details by memory or silos
- Surgeons walk into cases with incomplete or outdated plans
- Nurses delay prep while waiting for verbal confirmation
- Schedulers rearrange blocks manually like a game of Tetris
As surgical volume grows, cracks in the system widen. Without integration, ASCs hit a ceiling—they cannot scale without overwhelming their teams.
What True Integration Looks Like
Integration means systems that share data instantly and accurately across departments. In a fully integrated ASC:
- Data entered once populates everywhere it’s needed
- Clearances sync automatically from the EHR to the surgical schedule
- Consent forms, pre-op readiness, and post-op notes update in real time
- Clinics can submit ASC scheduling requests directly
Instead of people acting as bridges between tools, the system itself ensures clarity, visibility, and accountability.
Why Integration Matters
When workflows are fragmented, the costs are real:
- Staff burnout rises as nurses and admins chase paperwork instead of patients
- Patient experience suffers from delays, repeated questions, and disorganization
- Revenue is lost every time a case is delayed, canceled, or underutilized
You can’t grow surgical volume on a workflow that breaks under pressure. Integration is the infrastructure your ASC needs to deliver precision at scale.
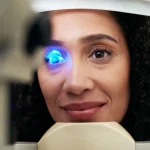
Introducing RetinaWise AI

RetinaWise AI is designed to solve these very challenges for ophthalmology ASCs. Unlike generic tools, it’s built for the unique demands of cataract, retina, glaucoma, and corneal surgery workflows.
- With RetinaWise AI, practices can:
- Eliminate redundant data entry across systems
- Ensure clearances, consents, and surgical plans sync automatically
- Gain real-time visibility into every case’s readiness
- Track pre-op, intra-op, and post-op workflows from one interface
- Reduce admin overhead while increasing throughput
The Gains from AI-Driven Integration
Adopting RetinaWise AI produces measurable improvements:
- Recovered Lost Case Volume – Prevent cancellations and delays caused by missing documentation, recapturing up to $150,000 annually.
- Increased Throughput Without Adding Staff – Add 1–2 more cases per OR day, driving $400,000–$800,000 in additional revenue.
- Reduced Admin and Overtime Costs – Save 8–10 hours per week of manual tracking and coordination, freeing staff to focus on patients.
- Improved Surgeon Efficiency – Minimize idle time, protecting $75,000–$100,000 annually in lost clinical productivity.
Why RetinaWise AI is Different
- Purpose-built for ophthalmology – Designed around real-world surgical workflows, not generic templates
- Seamless integration – Connects with EHR and admin systems for end-to-end workflow visibility
- Rapid adoption – Built to match how ophthalmology staff already work, reducing training time
- Scalable by design – Supports higher surgical volumes without burning out staff
- This isn’t just an efficiency upgrade—it’s the foundation for scalable, reliable surgical operations.
Build a Scalable Future for Your ASC
For ophthalmology practices, ASC integration isn’t optional. It’s the difference between running at 80% capacity with constant friction—or running at full precision, with room to grow.
RetinaWise AI provides the infrastructure for surgical reliability, efficiency, and growth.
Learn more about how RetinaWise AI can transform your surgical workflows: https://retinawiseai.com/ or Request a Free Demo